Introduction — a shift we can’t ignore
For decades, cancer has been framed in the public mind as a disease of older adults. That image is changing. Over the past two decades physicians and researchers in the United States have reported a steady rise in certain cancers among younger adults — most notably colorectal cancer — that has shifted the age distribution of diagnoses and raised alarm bells for clinicians, public-health officials, and young people alike. One widely cited analysis of hospital-based data found a 15% increase in colon cancer diagnoses among people aged 18–50 since 2004, a trend that deserves attention from patients, providers, and policymakers. (ACS)
This article explains what we know about cancer in younger adults, with a focus on colorectal cancer: how rates are changing, who’s affected, possible causes, early warning signs, diagnostics and screening developments, treatment implications, prevention strategies, and what patients and clinicians can do now. Wherever possible I cite the most reliable, recent sources so readers can follow up on the original studies and guidance. (American Cancer Society, PMC)
The data: numbers that changed the narrative
Multiple population- and hospital-based datasets show similar patterns: while overall cancer incidence and mortality have fallen in older adults for many cancer types thanks to better screening, treatment, and prevention, the incidence of colorectal cancer in adults younger than 50 has risen steadily. For example, national-level cancer surveillance and research analyses show increasing incidence rates in people under 50 over recent decades. In 2019 roughly 1 in 5 colorectal cancers were diagnosed in people aged 54 or younger — up from about 1 in 10 in the mid-1990s. (American Cancer Society, PMC)
The 15% figure (an increase in colon cancer diagnoses among ages 18–50 since 2004) comes from analysis of the National Cancer Database (NCDB) and related hospital-based datasets and has been summarized in clinical society communications. This is an important, load-bearing statistic because it quantifies the magnitude of change across a broad clinical population and underscores that the rise is not a niche or regional phenomenon. (ACS)
Other analyses show age-specific trends: a roughly 1–2% annual increase for certain younger age brackets over recent decades, with particularly steep rises in some subgroups (rectal cancer has risen faster than colon cancer in some reports). Taken together, the data show a consistent upward trend in early-onset colorectal cancer across multiple high-income countries, including the U.S. (ACS Journals, The Lancet)
Who is being affected?
Early-onset cancers are not restricted to a single demographic. Key patterns observed in U.S. datasets include:
- Age distribution: Most of the rise is seen in people under 50, with notable increases in the 20–39 and 40–49 subgroups. Some reports show 20–39 rising by ~1.6% per year since 2004 and faster annual increases for 40–44 in more recent years. (Fox News, Yahoo)
- Race and ethnicity: While colorectal cancer has traditionally impacted White adults at higher absolute numbers, relative increases in early-onset disease have been observed across racial and ethnic groups; outcomes (survival) still vary by race, reflecting disparities in access, stage at diagnosis, and comorbidities. (American Cancer Society, ACS Journals)
- Geography and socioeconomic status: Rising early-onset incidence has been reported nationwide but can concentrate in places with higher prevalence of obesity, poor access to preventive care, or lifestyle risk factors. Health-insurance status and screening access also shape diagnosis patterns. (American Cancer Society, CDC)
Importantly, many young adults diagnosed with colorectal cancer do not have familiar hereditary syndromes (like Lynch syndrome or familial adenomatous polyposis). While inherited cancer risk is important to evaluate, a large fraction of early-onset cases appear “sporadic” — meaning driven by other, possibly environmental or lifestyle-related causes. (PMC)

Why the rise? Leading hypotheses and what the evidence says
Medicine rarely finds a single cause for complex population shifts. For colorectal cancer in younger adults, several plausible drivers are under study:
- Changes in diet and food processing. The rise in ultra-processed food consumption, higher intake of red and processed meats, lower fiber intake, and greater sugar/fast-food consumption are consistent with known colorectal risk pathways (gut inflammation, microbiome shifts, obesity). Several public-health commentators point to the westernized diet as a likely contributing factor. (Cancer Research Institute, Women’s Health)
- Obesity and metabolic disease. The obesity epidemic has shifted population risk profiles. Obesity increases chronic inflammation and insulin resistance — both implicated in colorectal carcinogenesis. The timing of obesity increases across cohorts aligns plausibly with rising early-onset cancers. (Cancer Research Institute, American Cancer Society)
- Microbiome and antibiotic exposure. Changes in gut microbiota from early-life antibiotics, diet, or other exposures could promote carcinogenic processes. This is an active research area; while animal and mechanistic data are suggestive, human causality remains under investigation. (PMC)
- Sedentary lifestyles and low physical activity. Reduced physical activity increases colorectal risk; combined with diet and obesity this forms a plausible, multifactorial explanation. (Cancer Research Institute)
- Environmental exposures and unknown factors. Environmental carcinogens, endocrine disruptors, or exposures not yet identified might contribute. Researchers are cautious: current evidence does not isolate a single new carcinogen that explains the trend. (The Lancet, PMC)
- Detection artifacts? Some of the increase could reflect better imaging or incidental detection, but the rise in advanced-stage diagnoses among young adults argues against the idea that it’s only more testing finding harmless, early lesions. In fact, advanced-stage disease in younger people has increased in some datasets, which suggests a genuine rise in clinically significant cancer. (American Cancer Society, ACS Journals)
In short, the most likely explanation is multifactorial: changing lifestyles, population-level metabolic shifts, microbiome changes, and environmental exposures acting across birth cohorts. More research is urgently needed. (PMC, The Lancet)
Signs and symptoms every young adult should know
Early detection is crucial, especially because standard screening historically started at older ages. Common colorectal cancer signs and symptoms that should prompt medical attention (no matter your age) include:
- Persistent change in bowel habits (diarrhea, constipation, or narrowing of stools)
- Unexplained rectal bleeding or blood in the stool
- Persistent abdominal pain, cramps, or bloating
- Unexplained weight loss and fatigue
- A feeling that the bowel does not empty completely
It’s important: young age does not rule out colorectal cancer. If you experience any of the above symptoms lasting more than a few weeks, see a health professional and insist on appropriate diagnostic workup. Recent analyses show that younger patients often have symptoms that are initially dismissed or misattributed, causing delays in diagnosis and more advanced-stage disease at presentation. (American Cancer Society, PMC)
Screening: guidelines have changed — what that means
Historically, routine average-risk colorectal cancer screening began at age 50. In recent years, multiple professional bodies recognized rising early-onset incidence and recommended lowering the starting age:
- The American Cancer Society recommended lowering the starting age to 45 in 2018; the U.S. Preventive Services Task Force reaffirmed the move in 2021, recommending that routine screening begin at age 45 for average-risk adults. These shifts have increased screening uptake among 45–49-year-olds and are changing the landscape of early detection. (Wall Street Journal, Business Insider)
- Screening modalities include colonoscopy, stool-based tests (FIT, FIT-DNA), sigmoidoscopy (less common now), and CT colonography. For higher-risk individuals (family history, genetic syndromes, prior polyps), earlier and more frequent screening is indicated. (American Cancer Society)
Lowering screening age addresses part of the problem (45–49 benefit), but it does not solve the rising incidence in people younger than 45, which is where some of the sharpest increases have occurred. Therefore clinicians emphasize symptom awareness, risk assessment, and low-threshold diagnostic evaluation for symptomatic younger adults. (ACS Journals, PMC)
Diagnosis and treatment in younger patients — differences and challenges
Younger patients frequently present with more advanced or aggressive disease. Several challenges arise:
- Delay in diagnosis: Symptoms in young adults can be misattributed to hemorrhoids, irritable bowel syndrome, or infections — delaying referral for colonoscopy. Education for both patients and primary care clinicians is critical. (PMC)
- Aggressive tumor biology: Some evidence suggests that early-onset colorectal cancers can have adverse molecular features and occur at more advanced stages, necessitating multimodality treatment (surgery, chemotherapy, targeted therapy, sometimes immunotherapy). Outcomes vary by stage, tumor biology, and access to specialty care. (ACS Journals)
- Fertility and survivorship concerns: Younger patients face unique quality-of-life issues — fertility preservation, long-term chemotherapy effects, employment disruption, psychosocial stress, and financial toxicity. Oncologic care for younger adults often requires a multi-disciplinary approach that attends to these life-stage needs. (American Cancer Society)
- Genetic evaluation: Given the higher proportion of hereditary syndromes revealed in younger patients (though most are sporadic), referral for genetic counseling and testing is recommended when family history or tumor features suggest hereditary risk. (PMC)
Prevention: proven steps and practical advice
Prevention strategies that lower colorectal cancer risk also improve overall health. Recommendations include:
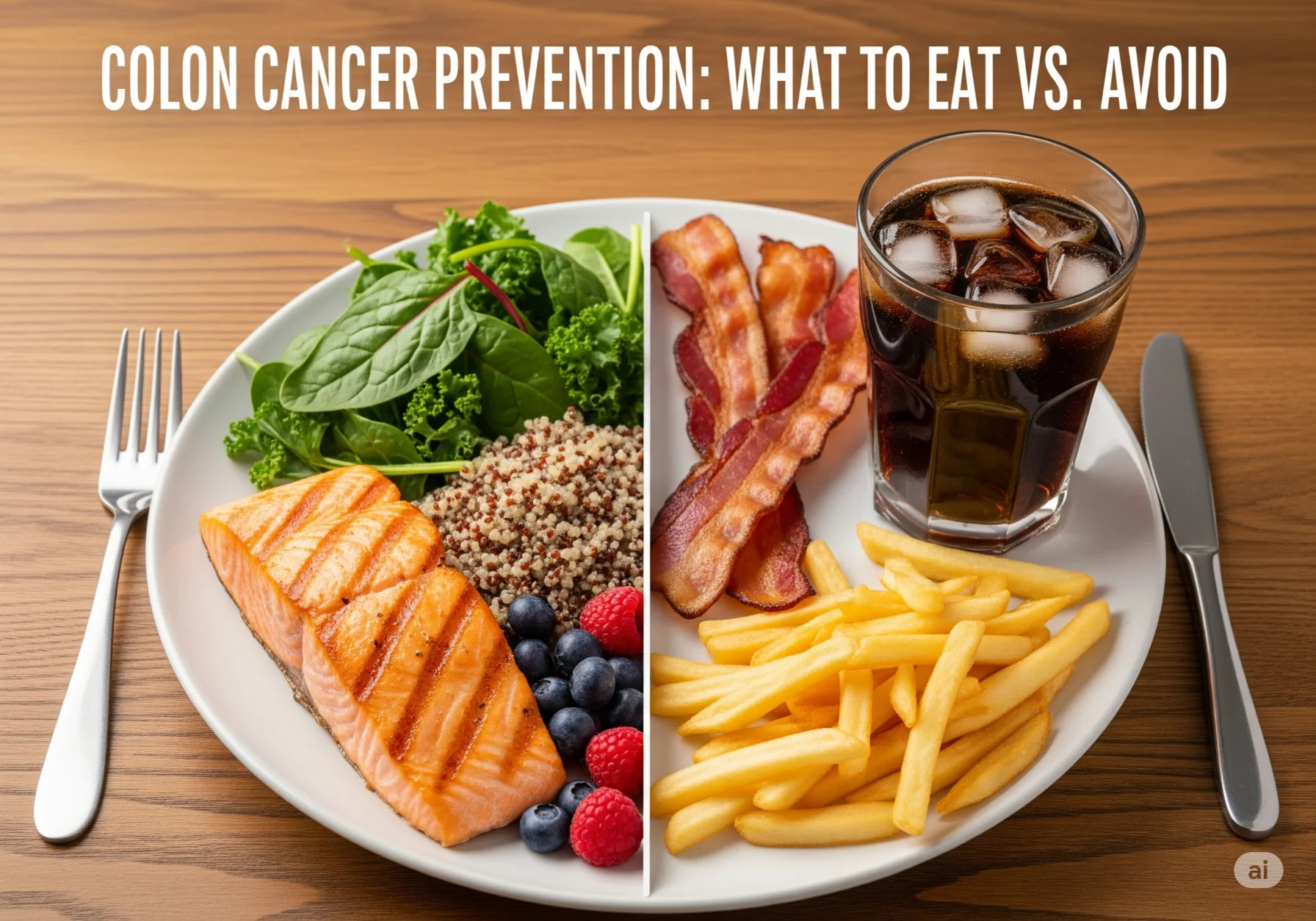
- Dietary patterns: Increase dietary fiber (fruits, vegetables, whole grains), reduce consumption of processed meats and excess red meat, avoid excessive ultra-processed foods and sugary beverages. (Cancer Research Institute)
- Maintain a healthy weight and be physically active: Achieve and maintain a healthy BMI, and aim for regular physical activity (150 minutes of moderate aerobic activity per week as a general public-health guideline). (American Cancer Society)
- Limit alcohol and stop tobacco: Both are established risk factors for multiple cancers including colorectal cancer. (PMC)
- Know your family history and discuss it with a clinician: A strong family history of colorectal or related cancers may require earlier or more intensive screening. Genetic counseling should be considered where appropriate. (PMC)
- Participate in recommended screening: If you’re 45 or older, follow current screening recommendations. If you’re younger but symptomatic or have a family history, seek evaluation without delay. (Wall Street Journal, American Cancer Society)
Prevention messaging should be culturally sensitive and feasible; public-health programs that make healthy food and active living easier are critical complements to individual choices.
Public health implications and system responses
Rising cancers in younger adults has broad implications:
- Health-system planning: Oncology services, survivorship programs, and fertility/psychosocial supports must be adapted to meet the needs of a younger, working-age patient population. (American Cancer Society)
- Screening policy: Lowering the screening age to 45 is an important policy step, but many unanswered questions remain: How to reach uninsured or under-screened populations? How to tailor screening for earlier ages? How to integrate stool-based testing at scale? (Business Insider, CDC)
- Research funding priorities: We need investments in etiologic research (diet, microbiome, environmental exposures), cohort studies of younger people, molecular characterization of early-onset tumors, and implementation science to improve screening uptake and equity. (The Lancet, PMC)
- Education and awareness: Both clinicians and the public need up-to-date information: clinicians to avoid dismissing red-flag symptoms in young adults; the public to recognize that colorectal cancer can occur at any adult age. Professional societies and advocacy groups are actively promoting awareness campaigns. (ACS, Cancer Research Institute)
Real-world cases: learning from data and stories
Clinical narratives and registry data illustrate the human impact behind the numbers: young parents diagnosed suddenly after months of symptoms, college students treated for advanced rectal cancer, and survivors navigating early menopause or infertility after treatment. While anonymized case vignettes can be powerful teaching tools, the broader lesson is systemic: timely access, rapid diagnostic pathways, and targeted support services can materially change patient outcomes.
Data-driven initiatives — such as mailed FIT testing, navigation programs for follow-up colonoscopy, and primary-care education — have shown improved screening uptake in younger age brackets when designed to reduce practical barriers (cost, time, fear). (Business Insider, American Cancer Society)
Practical checklist — what to do if you’re worried
If you’re a young adult concerned about colorectal cancer, use this practical checklist:
- Know the symptoms (change in bowel habits, bleeding, persistent abdominal pain, unexplained weight loss). If symptoms persist for more than 2–4 weeks, see a clinician. (American Cancer Society)
- Share your family history — cancers in first-degree relatives (parents, siblings) before age 60 or multiple relatives with colorectal or related cancers warrant earlier evaluation. (PMC)
- If you’re 45 or older, follow guideline screening (colonoscopy or stool-based testing). If you’re younger but have symptoms or risk factors, advocate for evaluation — don’t accept dismissal solely due to age. (Wall Street Journal, ACS Journals)
- Adopt risk-reducing behaviors: more whole foods and fiber, less processed foods and alcohol, maintain activity and healthy weight, and avoid tobacco. (Cancer Research Institute)
- Ask your clinician about referral to a gastroenterologist or genetic counselor if there’s concern. (PMC)
What clinicians and systems should do now
Clinical leaders and health systems can respond proactively:
- Lower barriers to diagnostic evaluation for symptomatic young adults (rapid-access colonoscopy pathways, triaged FIT testing). (Business Insider)
- Educate primary-care clinicians about rising early-onset colorectal cancer and provide clear symptom-to-workup algorithms. (PMC)
- Improve screening equity — implement outreach programs (mail FIT kits, community-based education), focusing on uninsured and historically under-screened populations. (Business Insider, CDC)
- Invest in research on causes and preventive interventions, with funds targeted to microbiome studies, diet and metabolic risk, and environmental exposures. (The Lancet)
A note on survival and hope
Colorectal cancer treatment has improved substantially over decades; when detected early, five-year survival rates are far better than for advanced disease. The trend toward earlier detection for 45–49-year-olds following guideline changes is encouraging — early-stage diagnosis is rising in that group. However, the continuing rise in incidence for those under 45 and the increase in advanced-stage disease among younger patients are sobering reminders that prevention and awareness must accelerate. (Wall Street Journal, American Cancer Society)
Final thoughts — shifting from alarm to action
Rising cancer rates in younger adults — especially the documented increase in colorectal cancer diagnoses among 18–50-year-olds — are a wake-up call. The numbers demand a three-part response:
- Personal vigilance: Know the symptoms, maintain healthy lifestyles, and get appropriate screening.
- Clinical vigilance: Clinicians must take young adults’ symptoms seriously and use available diagnostic tools without age bias.
- Public-health action and research: Policies that expand screening access, fund etiologic research, and support prevention programs must be prioritized.
This is not a cause for panic, but it is cause for focused, sustained action. Young adults, clinicians, researchers, and policymakers all have roles to play. Understanding how lifestyle, environment, biology, and healthcare access interact will be central to reversing these trends — and early detection remains our most immediate lever to save lives and preserve quality of life.
Key sources and further reading
(Selected authoritative sources cited in this article)
- American Cancer Society — Colorectal Cancer Facts & Figures 2023–2025. (American Cancer Society)
- PubMed Central review: Colorectal cancer in younger adults. (PMC)
- FACS press release summarizing NCDB finding of a 15% increase (people aged 18–50 since 2004). (ACS)
- Recent journal analyses and reviews on incidence trends (Lancet Oncology, Cancer journals). (The Lancet, ACS Journals)
- CDC United States Cancer Statistics (USCS) highlights. (CDC)






Leave a Reply