Introduction: The Digital Health Revolution
The past decade has brought healthcare into a new era—one where technology is no longer an accessory but a core driver of patient care. This shift accelerated dramatically during the COVID-19 pandemic, when healthcare providers were forced to adopt telehealth, digital health records, and remote patient monitoring almost overnight.
Yet the changes have proven not to be temporary. Digital health is here to stay, and interoperability—the ability of systems and devices to exchange and interpret shared data—is becoming the glue that holds this new model together.
From AI-powered diagnostics to real-time patient data sharing, the healthcare landscape is moving toward a future where patients experience seamless, personalized, and efficient care—whether they’re in a hospital, at home, or on the other side of the world.
The Permanence of Telehealth in Modern Care

Telehealth exploded in popularity during the pandemic, but data shows it’s not just a crisis tool—it’s becoming a permanent fixture in modern healthcare.
Key factors driving telehealth permanence:
- Convenience and Accessibility: Patients no longer need to travel long distances or sit in crowded waiting rooms for routine consultations.
- Cost Efficiency: Virtual visits can lower both provider and patient costs by reducing facility overhead and travel expenses.
- Better Access for Rural Communities: Areas with few specialists can now connect to top medical professionals globally.
- Integration with Wearables: Smart devices like blood pressure cuffs, glucose monitors, and heart rate trackers feed real-time data to clinicians during calls.
According to McKinsey, telehealth utilization is stabilizing at levels 38 times higher than pre-pandemic. Health systems now view it as a strategic service line rather than a stopgap solution.
Data-Sharing Standards: Breaking Down Silos

A critical barrier in healthcare’s digital transformation is the fragmentation of patient data. Historically, hospitals and clinics used proprietary electronic health record (EHR) systems that couldn’t “talk” to each other. The result? Patients might have bits of their medical history scattered across multiple platforms.
Interoperability aims to fix this by creating systems that exchange, interpret, and use health data universally.
Key Standards Driving Change
- HL7 (Health Level Seven): A long-standing framework for healthcare information exchange.
- FHIR (Fast Healthcare Interoperability Resources): A modern standard enabling easier, API-based data sharing.
- IHE (Integrating the Healthcare Enterprise): Profiles that define how to use existing standards in practical ways.
With governments, like the U.S. Office of the National Coordinator for Health Information Technology (ONC), pushing for open API access, patients now have more control over their data and providers have better tools for coordinated care.
AI Integration in Diagnostics and Care Delivery
Artificial Intelligence (AI) is redefining diagnostics, making processes faster, more accurate, and more predictive.
Examples of AI in healthcare:
- Radiology: AI algorithms can detect tumors, fractures, and abnormalities in medical imaging with accuracy rivaling human experts.
- Pathology: AI systems analyze biopsy slides for cancer detection.
- Predictive Analytics: AI can forecast patient deterioration or readmission risk.
- Virtual Health Assistants: Chatbots help triage symptoms, schedule appointments, and provide medication reminders.
A significant benefit of AI integration is decision support. Rather than replacing doctors, AI augments their expertise, enabling faster diagnosis and treatment planning.
Seamless Patient Experiences: The End Goal
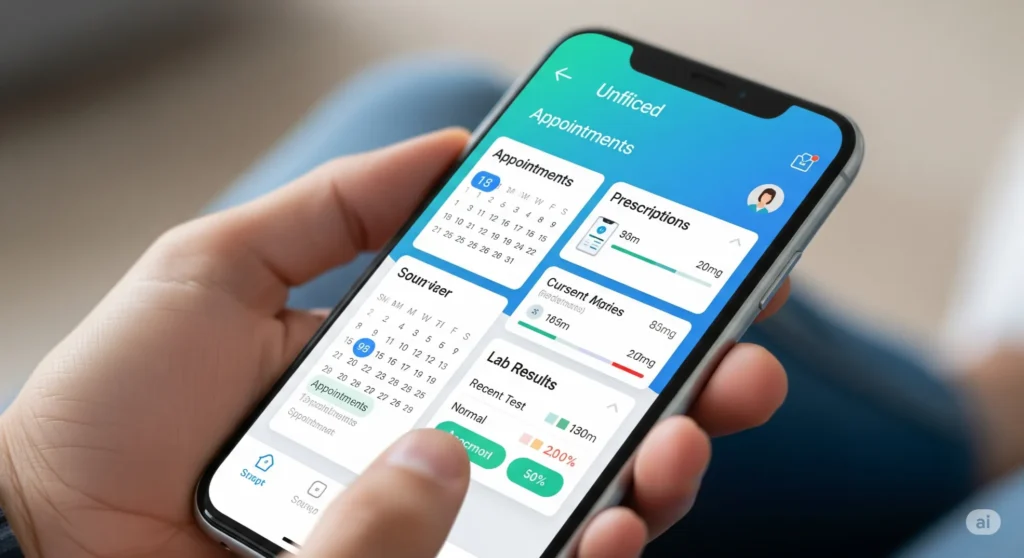
Healthcare has traditionally been disjointed—patients might need to log into multiple portals for test results, prescriptions, and appointments. The new vision is one unified experience where all health data and services live in a single platform.
Features of a truly seamless system:
- Unified Patient Records: All medical history accessible from one interface.
- Cross-Platform Apps: Mobile and desktop access without compatibility issues.
- Integrated Services: Appointment booking, telehealth calls, lab tracking, and prescription refills all in one place.
This not only improves convenience but also reduces medical errors caused by incomplete information.
Privacy, Security, and Ethical Considerations

The more interconnected healthcare becomes, the more cybersecurity and privacy take center stage.
Key Concerns:
- HIPAA Compliance: Ensuring data is protected in transmission and storage.
- Consent Management: Patients must control who can access their data.
- Data Breaches: Healthcare is a prime target for hackers due to sensitive personal information.
Ethical considerations extend beyond security to include AI bias, equitable access to digital tools, and preventing technology from widening health disparities.
The Role of Government and Policy
Governments play a pivotal role in accelerating or slowing interoperability.
Notable policy drivers:
- 21st Century Cures Act (U.S.): Mandates open APIs for health data sharing.
- EU eHealth Digital Service Infrastructure: Enables cross-border health record sharing in Europe.
- Incentives for Interoperability Compliance: Funding programs for hospitals that meet integration benchmarks.
Without policy alignment, interoperability risks stalling due to vendor lock-in and incompatible systems.
Case Studies and Success Stories
Example 1: Kaiser Permanente
Kaiser achieved near-complete EHR interoperability across its network, allowing instant data sharing among physicians, pharmacists, and specialists.
Example 2: NHS Digital (UK)
Implemented FHIR-based APIs to enable different NHS trusts to exchange patient data, improving emergency care outcomes.
The Road Ahead: Trends to Watch

Emerging trends include:
- Real-Time Remote Monitoring: Wearables providing continuous health metrics to providers.
- Personalized AI-Driven Care: Tailoring treatments based on genetic, lifestyle, and historical health data.
- Global Interoperability: Systems that work across borders for traveling patients and global health crises.
Conclusion: Building a Connected, Patient-Centered Future
The future of healthcare is connected, intelligent, and patient-first. Digital health and interoperability are not just technological shifts—they are cultural transformations that redefine how care is delivered, experienced, and improved.
Patients will soon expect frictionless access to their entire health journey, while clinicians will have unprecedented insight into patient needs. For this future to materialize, collaboration between technology providers, healthcare institutions, and governments is essential.
The journey toward true interoperability is complex, but the reward—a world where healthcare is efficient, equitable, and deeply personalized—is well worth the effort.






Leave a Reply