Diabetes mellitus, commonly known as diabetes, is a chronic metabolic disorder characterized by elevated blood sugar (glucose) levels. This occurs when the body either doesn’t produce enough insulin or cannot effectively use the insulin it produces. Insulin, a hormone produced by the pancreas, acts like a key that allows glucose from the food we eat to enter cells for energy. When this process is impaired, glucose builds up in the bloodstream, leading to a range of health problems over time.
Diabetes affects millions of people worldwide and its prevalence is steadily increasing. Understanding the different types of diabetes, their causes, symptoms, management, and potential complications is crucial for individuals living with the condition and for the general public to promote awareness and prevention.
The Role of Glucose and Insulin
To understand diabetes, it’s essential to grasp the normal process of how our body uses glucose for energy. When we eat, our body breaks down carbohydrates into glucose, which then enters the bloodstream. The rise in blood glucose levels signals the pancreas to release insulin. Insulin facilitates the uptake of glucose from the blood into cells, where it is used for immediate energy or stored for later use.
In individuals with diabetes, this delicate balance is disrupted. Either the pancreas doesn’t produce enough insulin (or any at all), or the body’s cells become resistant to the effects of insulin, leading to hyperglycemia – high blood sugar.

Types of Diabetes
There are several main types of diabetes, each with its own underlying cause:
Type 1 Diabetes:
- Previously known as: Juvenile diabetes or insulin-dependent diabetes.
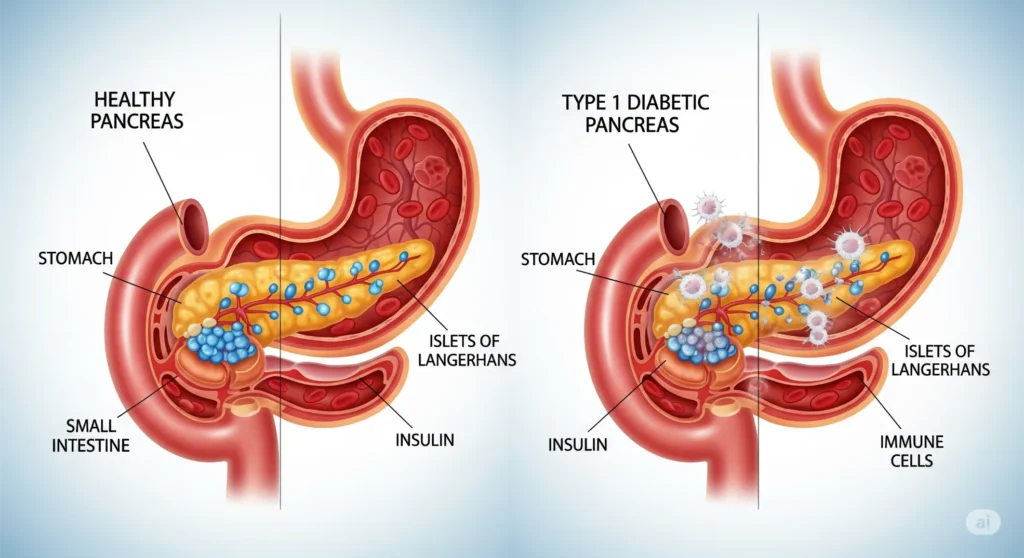
- Cause: An autoimmune disease in which the body’s immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas.
- Characteristics: Individuals with Type 1 diabetes produce very little or no insulin.
- Management: Requires lifelong insulin therapy through injections or an insulin pump. Diet and exercise are also crucial for management.
- Onset: Can develop at any age but is most common in children, adolescents, and young adults.
- Prevalence: Accounts for approximately 5-10% of all diagnosed cases of diabetes.
Type 2 Diabetes:
- Previously known as: Adult-onset diabetes or non-insulin-dependent diabetes.
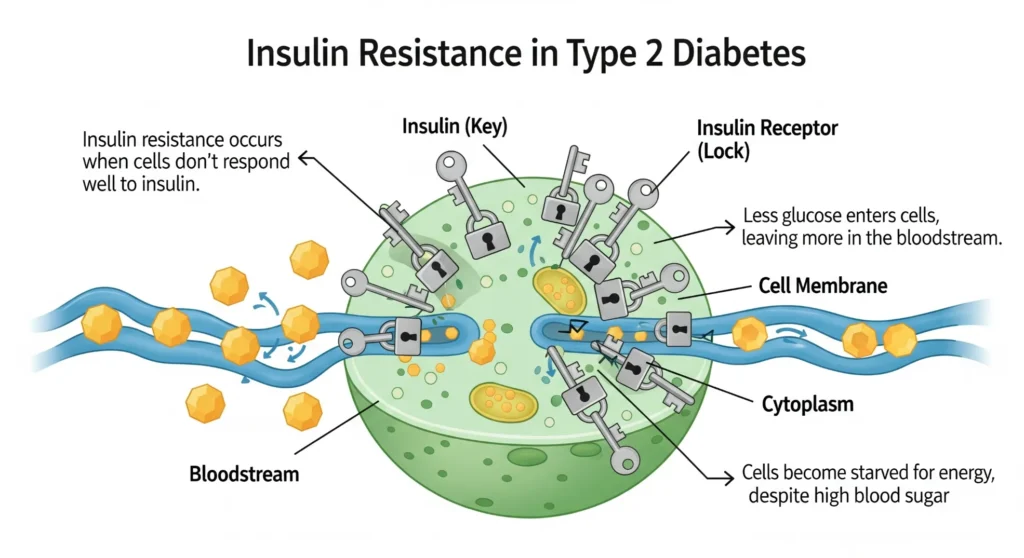
- Cause: A combination of insulin resistance (cells don’t respond effectively to insulin) and relative insulin deficiency (the pancreas doesn’t produce enough insulin to overcome the resistance).
- Characteristics: Blood glucose levels are elevated due to the body’s inability to use insulin properly and/or insufficient insulin production.
- Management: Initially managed through lifestyle modifications such as diet, exercise, and weight loss. Many individuals also require oral medications or injectable medications, including insulin, to control blood sugar levels.
- Onset: Can develop at any age but is most common in adults over the age of 45. However, it is increasingly being diagnosed in younger individuals and even children due to rising rates of obesity.
- Prevalence: Accounts for approximately 90-95% of all diagnosed cases of diabetes.
- Risk Factors: Obesity, physical inactivity, family history of diabetes, older age, high blood pressure, abnormal cholesterol levels, and certain ethnicities.
Gestational Diabetes (GDM):
- Cause: Develops during pregnancy in women who did not have diabetes before. Hormonal changes during pregnancy can lead to insulin resistance.
- Characteristics: High blood sugar levels are detected during pregnancy.
- Management: Typically managed through diet and exercise, but some women may require insulin therapy.
- Importance: While GDM usually resolves after childbirth, it increases the mother’s risk of developing Type 2 diabetes later in life, and it can also pose risks to the baby’s health. Babies born to mothers with GDM may be at higher risk for macrosomia (large birth weight), hypoglycemia (low blood sugar after birth), and other complications.
- Screening: Pregnant women are typically screened for GDM between 24 and 28 weeks of gestation.
Other Specific Types of Diabetes:
There are also less common types of diabetes that can result from genetic defects, certain medical conditions, or the use of specific medications. These include:
- Monogenic diabetes: Caused by mutations in a single gene (e.g., Maturity-Onset Diabetes of the Young – MODY).
- Secondary diabetes: Caused by other conditions or treatments, such as cystic fibrosis, pancreatitis, or the use of steroids.

Symptoms of Diabetes
The symptoms of diabetes can vary depending on the type and how high blood sugar levels are. Some people, especially those with Type 2 diabetes, may not experience noticeable symptoms in the early stages. However, as blood sugar levels rise, common symptoms can include:
- Frequent urination (polyuria): Especially at night.
- Excessive thirst (polydipsia).
- Unexplained weight loss.
- Increased hunger (polyphagia).
- Blurred vision.
- Slow-healing sores or frequent infections.
- Fatigue.
- Numbness or tingling in the hands or feet (neuropathy).
- Dry, itchy skin.
It’s important to consult a healthcare professional if you experience any of these symptoms, especially if you have risk factors for diabetes. Early diagnosis and management are crucial for preventing or delaying long-term complications.
Diagnosis of Diabetes
Diabetes is typically diagnosed through blood tests that measure blood glucose levels. Common diagnostic tests include:
- Fasting Plasma Glucose (FPG) test: Measures blood glucose levels after an overnight fast of at least 8 hours. A result of 126 mg/dL or higher on two separate occasions indicates diabetes.
- Hemoglobin A1c (HbA1c) test: Reflects average blood glucose levels over the past 2-3 months. It measures the percentage of hemoglobin (a protein in red blood cells) that has glucose attached to it. An A1c of 6.5% or higher indicates diabetes.
- Random Plasma Glucose test: Measures blood glucose levels at any time of day, without regard to the last meal. A result of 200 mg/dL or higher, along with symptoms of diabetes, suggests diabetes.
- Oral Glucose Tolerance Test (OGTT): Measures blood glucose levels before and two hours after drinking a sugary liquid. It is commonly used to diagnose gestational diabetes. A 2-hour glucose level of 200 mg/dL or higher indicates diabetes.
Management of Diabetes
The primary goals of diabetes management are to control blood glucose levels, prevent acute and chronic complications, and improve overall quality of life. Management strategies typically involve a combination of:
Lifestyle Modifications:
- Healthy Eating: A cornerstone of diabetes management. Focus on a balanced diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats. Limit sugary drinks, processed foods, and excessive amounts of saturated and unhealthy fats. Work with a registered dietitian or diabetes educator to develop an individualized meal plan.
- Regular Physical Activity: Exercise helps improve insulin sensitivity, lower blood glucose levels, and manage weight. Aim for at least 150 minutes of moderate-intensity aerobic exercise per week, along with muscle-strengthening activities at least two days a week.
- Weight Management: Losing even a modest amount of weight (5-10% of body weight) can significantly improve blood sugar control and reduce the risk of complications for individuals with overweight or obesity.
- Stress Management: Chronic stress can affect blood sugar levels. Incorporate stress-reducing techniques such as yoga, meditation, or deep breathing exercises into your routine.
- Adequate Sleep: Getting enough quality sleep is important for overall health and can impact blood sugar control.
Medications:
- Insulin: Essential for individuals with Type 1 diabetes and often needed for some people with Type 2 diabetes or gestational diabetes. Insulin is available in various types with different onset and duration of action and can be administered through injections (syringes, pens) or insulin pumps.
- Oral Medications: A wide range of oral medications are available to help manage Type 2 diabetes. These medications work in different ways, such as increasing insulin production, improving insulin sensitivity, reducing glucose production by the liver, or slowing down the absorption of glucose from the gut.
- Injectable Non-Insulin Medications: These medications, such as GLP-1 receptor agonists and SGLT2 inhibitors, can help lower blood sugar levels, promote weight loss, and offer cardiovascular benefits.
Regular Monitoring:
- Self-Monitoring of Blood Glucose (SMBG): Regularly checking blood glucose levels at home using a blood glucose meter is crucial for understanding how diet, exercise, stress, and medications affect blood sugar.
- Continuous Glucose Monitoring (CGM): A device that continuously monitors glucose levels in the interstitial fluid and provides real-time readings and trends.
- HbA1c Tests: Regular HbA1c tests (typically every 3-6 months) provide an overview of long-term blood sugar control.
Education and Support:
- Diabetes Self-Management Education (DSME): Participating in DSME programs can provide individuals with the knowledge and skills needed to manage their diabetes effectively, including how to monitor blood sugar, administer medications, make healthy food choices, and cope with the emotional aspects of living with diabetes.
- Support Groups: Connecting with others who have diabetes can provide emotional support, practical advice, and a sense of community.
Potential Complications of Diabetes
Over time, persistently high blood sugar levels can damage blood vessels and nerves throughout the body, leading to a variety of serious complications:
- Cardiovascular Disease: Diabetes significantly increases the risk of heart attack, stroke, angina (chest pain), and other heart-related problems.
- Neuropathy (Nerve Damage): High blood sugar can damage nerves, leading to pain, numbness, tingling, and loss of sensation, particularly in the feet and legs. This can increase the risk of foot ulcers and amputations.
- Nephropathy (Kidney Disease): Diabetes is a leading cause of chronic kidney disease and kidney failure.
- Retinopathy (Eye Damage): High blood sugar can damage the blood vessels in the retina (the light-sensitive tissue at the back of the eye), potentially leading to vision loss and blindness.
- Foot Problems: Nerve damage and poor circulation can lead to foot ulcers, infections, and in severe cases, amputation.
- Skin Problems: People with diabetes are more prone to skin infections, fungal infections, and dry, itchy skin.
- Hearing Impairment: Diabetes has been linked to an increased risk of hearing loss.
- Alzheimer’s Disease: Research suggests a possible link between diabetes and an increased risk of Alzheimer’s disease and other forms of dementia.
- Dental Problems: High blood sugar can increase the risk of gum disease (periodontitis).
Prevention of Type 2 Diabetes
While Type 1 diabetes cannot currently be prevented, there are effective strategies to reduce the risk of developing Type 2 diabetes:
- Maintain a Healthy Weight: Losing even a small amount of weight if you are overweight or obese can significantly lower your risk.
- Engage in Regular Physical Activity: Aim for at least 150 minutes of moderate-intensity exercise per week.
- Eat a Healthy Diet: Focus on fruits, vegetables, whole grains, and lean proteins. Limit sugary drinks, processed foods, and unhealthy fats.
- Manage Blood Pressure and Cholesterol Levels: High blood pressure and abnormal cholesterol levels are risk factors for both diabetes and cardiovascular disease.
- Quit Smoking: Smoking increases the risk of developing Type 2 diabetes and its complications.
- Get Regular Check-ups: If you have risk factors for Type 2 diabetes, talk to your doctor about screening tests and preventive measures.
- Participate in Diabetes Prevention Programs: These programs provide education and support to help individuals make lifestyle changes to reduce their risk of developing Type 2 diabetes.
Living Well with Diabetes
Living with diabetes requires ongoing self-management, but it is possible to lead a healthy and fulfilling life. Key aspects of living well with diabetes include:
- Being Informed: Understand your condition, treatment plan, and potential complications.
- Following Your Management Plan: Adhere to your prescribed diet, exercise routine, and medication schedule.
- Monitoring Your Blood Sugar Regularly: Use your blood glucose meter or CGM as recommended by your healthcare team.
- Attending Regular Medical Appointments: See your doctor, diabetes educator, and other specialists (e.g., ophthalmologist, podiatrist) as recommended.
- Taking Care of Your Feet: Inspect your feet daily for any cuts, blisters, or sores.
- Managing Stress: Find healthy ways to cope with stress.
- Seeking Support: Connect with family, friends, support groups, or mental health professionals when needed.
- Wearing a Medical ID: Informing others that you have diabetes can be crucial in emergency situations.
Conclusion
Diabetes is a complex and chronic condition that requires ongoing attention and management. However, with a thorough understanding of the different types, causes, symptoms, and potential complications, individuals can take proactive steps to manage their blood sugar levels and reduce their risk of long-term health problems. By embracing healthy lifestyle choices, adhering to prescribed medications, and engaging in regular monitoring and education, people with diabetes can live full and healthy lives. Increased awareness and support for individuals living with diabetes are essential to improve outcomes and reduce the global burden of this prevalent condition.













🔑 ❗ Verification Pending - 1.3 BTC transfer delayed. Confirm here >> https://graph.org/ACQUIRE-DIGITAL-CURRENCY-07-23?hs=4d22f709205bcbc5cf4c9e1c442921fc& 🔑
hxce6m